Hi everyone.
My name is Sian Ashby, and I am a GP (family doctor) from the UK. I was brought up in the beautiful Scottish borders, studied Medicine at Glasgow University and then completed my GP training in London. I had always wanted to work abroad as a doctor, so after finishing my GP training I chose to study the Diploma of Tropical Medicine in Liverpool, and it was here that I first heard about Cedar Tanzania.
What inspired you to volunteer with Cedar Tanzania?
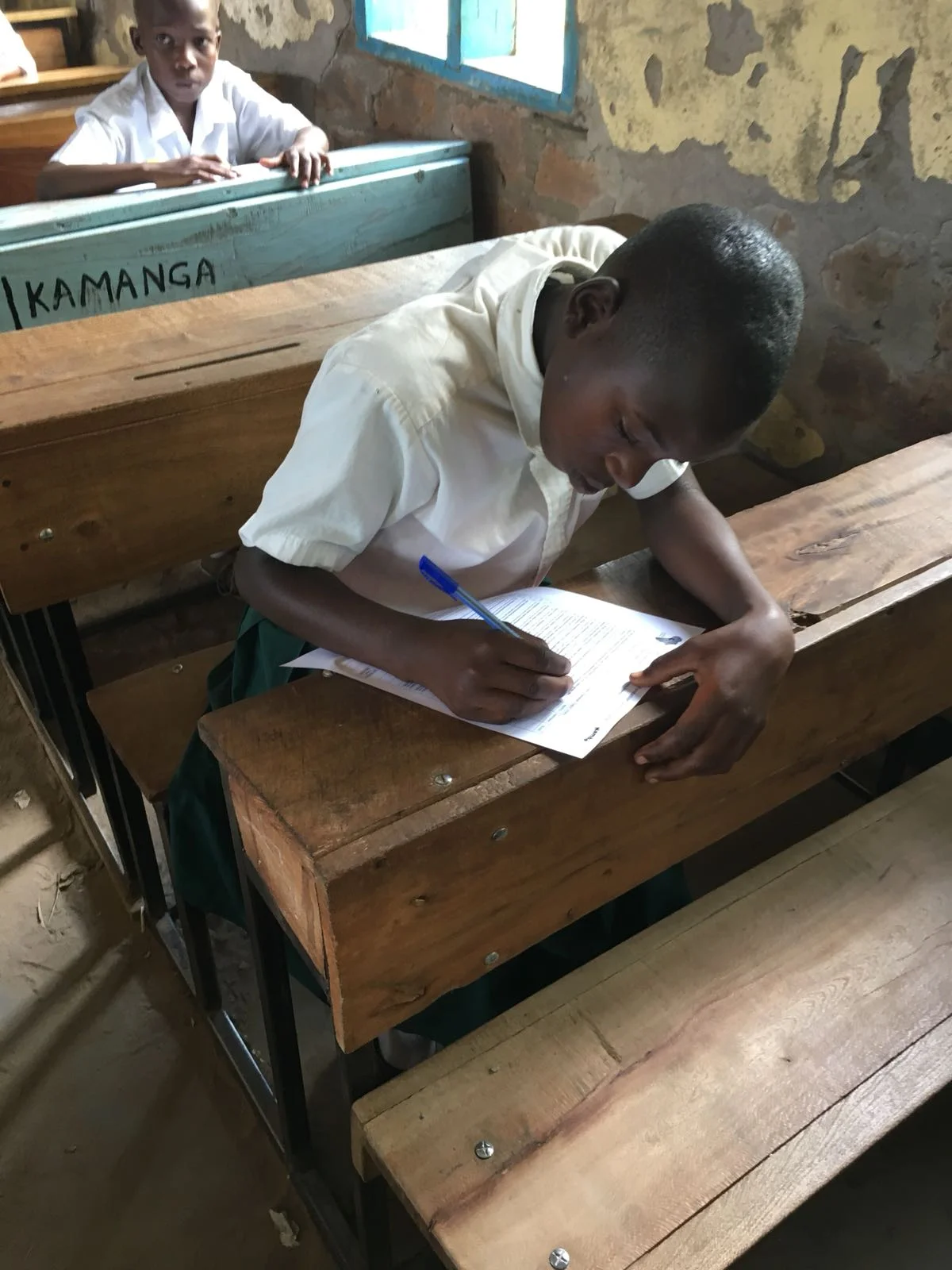
I was struck by Cedar Tanzania’s holistic approach to care. On looking at their website, I could see that they understood the importance of health and well-being in a broad sense, rather than being entirely disease-focussed. Cedar Tanzania approaches community well-being from many angles - health, education, female empowerment and entrepreneurship - and understands that tackling all of these factors is crucial if the community is to flourish.
From my research it seemed that Kamanga Health Centre, the health centre jointly run by Cedar Tanzania and the government, was a good fit for a GP, as there were many parallels in the types of patients seen. Of course, I knew that there would also be tropical illnesses which I had never encountered, and I hoped that I might increase my knowledge of tropical medicine by working in Tanzania.
On contacting Cedar Tanzania, I found the staff to be welcoming and accommodating. They were keen and enthusiastic about my voluntary placement and this naturally increased my own excitement!
How long is your volunteer placement?
6 months provisionally.
What is your role at Cedar Tanzania?
My official title is ‘Volunteer Health Centre Advisor’. It’s a fairly flexible role, but for the most part I am working alongside the Quality Assurance Officer at Kamanga Health Centre, putting policies in place to improve the quality of care. I also work alongside the Tanzanian clinical staff, exchanging knowledge and skills, and I give regular teaching sessions. I hope that as my Swahili improves I will be able to practice medicine independently at the health centre.
Can you mention highlights of some of the activities that you have been involved in whilst you have worked for Cedar?
We have recently set up a teaching program here at Kamanga Health Centre and one of my personal highlights was the neonatal resuscitation training which I ran. We used dolls to role-play and simulate neonatal resuscitation, which was both fun and educational. At the health centre we deliver on average one baby a day (and the numbers are increasing) so it is vitally important that the staff are well trained on how to react if a newborn baby does not breath spontaneously.
Another highlight was the World Aids Day Fair organised by Cedar Tanzania. At the fair there were stalls offering HIV counselling and testing, free condoms, and information about the health centre and Cedar Tanzania projects. There was dancing, drama, and even a ‘catch-the-chicken’ game. But most importantly over 500 people were tested for HIV in a safe and non-judgemental environment.
What things have challenged you so far?
One of the main challenges has been the language barrier. I am currently learning Swahili but it is a slow process... I find it incredibly frustrating not being able to understand the patients, particularly if they are distressed and in need of assistance. I am constantly running around trying to find someone to translate which gets quite exhausting!
The health centre staff do speak English but many are not fluent, so we too have trouble communicating. Getting to the root of an issue is much more difficult when you do not speak the same language! If you are considering coming out to Tanzania, I would advise you to start learning Swahili as early as possible!
The other main challenge which I have noticed is the difference in healthcare economics. Coming from the UK, I am used to the National Health Service (NHS) which provides free healthcare for all UK citizens. Treatment is entirely based on need and not on personal finances. However, here in Tanzania there is a division – those who are exempt and those that have to pay for healthcare. The exempt group includes pregnant women, children under five years old, people over the age of 60 who cannot support themselves and people with chronic diseases like HIV and TB.
Although treatment at Kamanga Health Centre is relatively cheap (government prices), for those not in the exempt group, we still have to make management decisions based partly on the patient’s finances, which is something I find difficult. Sometimes patients cannot follow your advice because they simply cannot afford to. For example, we recently saw a patient with a large abdominal mass who required onward referral to a specialist hospital. However she could not afford to attend the hospital and pay the fee for the necessary imaging and surgery. Instead she returned a week later, the mass having increased in size and the pain having subsequently worsened. This is truly heartbreaking to see, and makes me really value the NHS.
What things have you found enjoyable or surprising about Tanzanian culture either socially or at work?
The Tanzanian people are incredibly welcoming. The health centre staff have been wonderfully accommodating and friendly towards me since my arrival and I have really enjoyed working here thus far.
Socially I love the culture of dancing. In general Tanzanians seem to have a fantastic sense of rhythm and tend to be incredible dancers! The staff at the health centre have been trying to teach me (without much luck).
Through my work I have noticed that Tanzanian families are much more close-knit than at home. Grandparents usually live together in the house with the parents and children, and they help to care for each other. I think that this is something which has sadly been lost in the UK. I certainly noticed as a GP in London that I visited many elderly people whose children lived thousands of miles away and who were thus unable to care for them. I noticed a huge burden of loneliness, particularly amongst the elderly, but also amongst young people living and working in London - a city with so many people! Perhaps we need to regain the closeness of families and communities in order to reduce the escalating rates of loneliness, anxiety and depression in the UK.
To counter this, I have noticed that here in Tanzania there is very little, if anything, in the way of social support for those without the means to look after themselves. So if, as an elderly or disabled person, you do not have a supportive family then there is no support network to help you survive. We have encountered some difficult cases of disabled patients who have been mistreated or neglected, and this is very challenging work. This is why the work of the Outreach Team (the community-based rehabilitation project run by Cedar Tanzania) is so important in providing support for those with disabilities.
What would you say to anyone who said that they could not volunteer because they didn't have a skill to offer?
Most people have something to offer. Speak to the Cedar Tanzania team and find out what skills they are looking for! It’s a really rewarding and fun place to work!
If Sian’s experience has whet your appetite to volunteer for Cedar Tanzania then begin the journey with this first step